Cancer is a truly terrible disease, and although our ability to treat and even cure many types of cancer has greatly improved, our current methods for dealing with it are admittedly imperfect and often have serious side-effects. It is, therefore, hardly surprising that many people who are diagnosed with cancer would forgo science-based treatments for “alternative” or “complimentary” treatments (aka CAM). After all, who wouldn’t be tempted by the promise of a miracle cure? The problem is that these “natural” treatments are unproven and unregulated, and choosing them over science-based medicine actually increases your risk of dying from cancer. This was demonstrated by a paper published earlier this year (Johnson et al. 2018a) that compared people who took only alternative cancer treatments to those who took conventional treatments. It found that those who relied on alternative treatments had a significantly lower survivorship. A second study (by some of the same authors as the first study) was just published and further supports that conclusion, so I want to talk about it for a minute.
This study (Johnson et al. 2018b) differed from the previous study in that all of the patients used at least one round of conventional treatment, but some of them also used alternative treatments. To compare these groups, authors used a design known as a retrospective cohort study. I discussed this design at length here, but in brief, this means that the researchers took the medical records for a large group of people who had cancer, and the went through the records and split them up into a group that only reported using conventional treatments and a group that used at least some alternative treatments. Because this study design is entirely observational and these groups weren’t assigned beforehand, there were potential confounding factors. Therefore, the authors matched patients such that for every one person who used alternative treatments, there were four people who were similar in age, ethnicity, cancer type, cancer stage, etc. but used only conventional treatments. This resulted in the groups being as similar as possible for all confounding factors so that causation could be assigned.
They used a couple of different methods to analyze the data, but the core analyses were hazard ratios. The simplest way to think about this is that it is the hazard associated with one group divided by the hazard associated with the other group. Thus, a hazard ratio of 2 means that one group has twice the hazard as the other. In other words, if the outcome of interest is death, then all else being equal, you’d expect one group to have twice the rate of mortalities as the other at any given time point during the study. The actual math there gets a bit complicated because you need to use models that take into account confounding factors, but that’s the idea in a nutshell (note that this is not a measure of absolute risk).
So, what did this study find? There are several interesting results. First, people who used alternative treatments were less likely to use the full rounds of conventional treatments. In other words, many people were choosing alternatives instead of using the recommended schedule of conventional treatments.
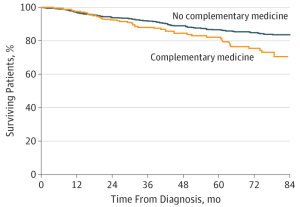
Figure 1 from Johnson et al. 2018b showing the difference in survivorship between those who did and did not use alternative cancer treatments.
The second key result was that the mortality rates were higher for people who used alternative treatments. The hazard ratio was 2.08 with a 95% confidence interval of 1.50–2.90. That result was based on a test that did not account for differences in the levels of conventional treatments that were used, and the authors followed up on it by doing a test that incorporated the history of conventional treatments. That second model showed no statistically significant difference between the two groups. This suggests that the increased mortality for people who used alternative treatments was driven by skipping conventional treatments rather than by the alternative treatments themselves. Thus, using the full course of conventional treatments was the key factor for maximizing survival.
So, does this mean that it is fine to take alternative treatments as long as you also take the full line of conventional treatments? Not necessarily. For one thing, there is no proven benefit from those alternatives. Further, out of necessity, this study lumped all alternative treatments together. As a result dangers of particular treatments may have been masked by a large number of benign treatments. Some alternatives are clearly dangerous (like drinking bleach and paint thinner), and others may be harmful on their own or have negative interactions with science-based treatments. We simply don’t know.
Risk assessment always has to weigh the benefits against the risks, and given that there are no known benefits of these alternative treatments, in my opinion, the risk and wasted money is not worth it. Having said that, as long as you are following the convention treatment schedule it is entirely possible that taking alternatives won’t do any harm (other than to your wallet), but at the very least tell your doctor exactly what you are taking and make sure that they don’t have reason to think that your chosen complementary “medicine” isn’t dangerous.
Finally, I want to talk about an important weakness of this study. Namely, the fact that, as I just stated, they lumped all alternative treatments together. This was out of necessity because there are a mind-boggling number of alternative treatments out there, and they only had 258 people in the alternative treatment group. Thus, there simply wasn’t enough power to test any particular alternative remedy. Further, beyond the dizzying array of alternatives available, for a study, you’d also need information about doses, schedules of administration, etc. In other words, the data simply aren’t there to do a comparison based on specific treatments. As a result, you could try to argue that your specific preferred alternative works, and it just couldn’t be detected because of all the statistical noise from the treatments that don’t work. It is technically possible that there were a few effective treatments in there, but that’s a dice-roll. It’s exactly the same as what I described earlier for risks. There may be a few good treatments in the mix, there may be some very harmful ones, there’s probably lots of neutral ones, and without properly controlled studies, you have no way of knowing which treatment is which. They all have anecdotes “supporting” them, and for any one of them you can find countless blogs, forums, etc. singing their praises, and you have no objective way of which ones (if any) are actually safe and beneficial. That’s why we have to rely on science, and why I don’t recommend that anyone take these untested treatments.
In short, replacing science-based cancer treatments with alternative or complementary treatments reduces your chance of survival, and you should not rely on them.
Related posts
- 5 reasons why anecdotes are totally worthless
- If anecdotes are evidence, why aren’t you drinking paint thinner?
- If cannabis and vitamin B17 kill cancer, why aren’t they approved by the FDA? Let me explain
- No one is hiding a cure for cancer
- Understanding the reported risks of medicines, foods, toxic chemicals, etc.
Literature cited
- Johnson et al. 2018a. Use of Alternative Medicine for Cancer and Its Impact on Survival. Journal of the National Cancer Institute 110:121–124.
- Johnson et al. 2018b. Complementary Medicine, Refusal of Conventional Cancer Therapy, and Survival Among Patients With Curable Cancers. JAMA
It is not clear from the report if the study subjects were matched for stage and type of cancer. If the cancer was diagnosed at a late stage or was a type for which there were no good science based treatments known it would not seem unlikely that the subject might take “nothing to lose” view and select alternative treatments which might be expected to lead to poor outcome due to the condition of the subject rather than the treatment. This would make it hard to interpret the data.
LikeLike
This was accounted for in the study.
From the methods section describing their matching prototypical, “matching was based on variables identified a priori to be of interest, including age, clinical group stage, Charlson-Deyo comorbidity score, insurance type, race/ethnicity, year of diagnosis, and cancer type.”
Also, in the results section, they say that in their statistical models they controlled for, “age, cancer type, sex, race/ethnicity, income, educational level, residence setting, geographic area, insurance type, facility type, clinical stage and comorbidity score”
LikeLike